Blood Types in Humans and Our Canine Companions
Blood Typing in Dogs
by Meg Hamill
Bachelor of Biomedical Science
Deakin University
Do you know your blood type? At some stage in our lives, most people would have been made aware of their blood type, whether it be from a blood test or if they have donated blood, but do you know what this actually means? What is the difference between people with differing blood types?
In this article I will explore what blood actually is, and what component of our blood that is the marker that determines our blood type. I will discuss the ABO and Rhesus blood typing systems used in humans, then compare this with the blood typing systems used in dogs. Lastly, I will explain why it is important for us to know both our blood type as well as our dogs blood type.
How do we determine blood types?
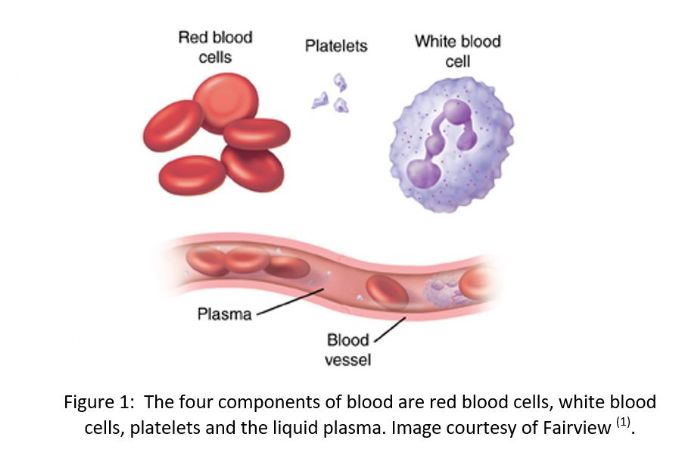
Blood is a body fluid that is composed of four main components. There are red blood cells (erythrocytes) that carry oxygen around the body, white blood cells (leukocytes) that protect the body from infection and platelets that help form a blood clot when there is injury. The fourth component is the liquid component plasma which transports the other blood cells as well other important molecules such as hormones, electrolytes and proteins through the body (1). A single human red blood cell is approximately 8 µm (.008 mm) in diameter and 2 µm (.002 mm) thick and we have on average 5 billion of them for every ml of blood. This means that with the 5L of blood we have in our body, we have around 2.5 x 1013 (25,000,000,000,000) red blood cells (2)!
A person’s blood type is identified by the presence or absence of certain molecules (antigens) on the surface of their red blood cells. So what is it that makes red blood cells different in different people? It is the presence of small sugars or proteins called antigens that are attached to the cell membrane of the red blood cells. (3). It is by identifying these antigens that we are able to determine blood type using the ABO and Rhesus blood typing systems.
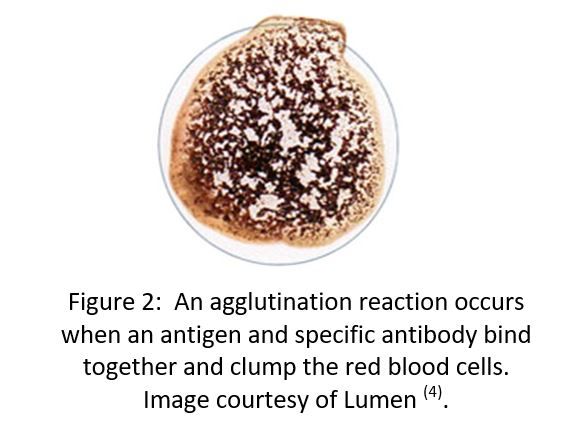
To test for blood type, a blood sample is mixed with a known antibody to see if a reaction occurs. Antibodies will bind specifically to the corresponding antigen on the surface of the red blood cell to form a characteristic “clumping” reaction know as an agglutination reaction.
For example, if a person with blood type A has a sample of their blood mixed with antibody to Group A an agglutination reaction will occur. This clumping is shown in the image below.
The antigens present on the surface of human red blood cells that are used to determine blood type are A and B antigens (3). People will either have only A, only B, both A and B or neither A or B on the surface of their cells. The agglutination reaction indicates the presence of the antigen type, and the antigen type determines a person’s blood type.
For example, if a person has A antigens on their red blood cells, they are blood group A, if they have both A and B antigens on their red blood cells, they are blood group AB, and if they have no antigens on their red blood cells, they are blood group O. Refer to your table here?
People also have antibodies in their plasma that act as part of the bodies defence system to recognize and attack anything that is foreign in the blood stream. Antibodies are very specific for their antigen. In healthy people our immune system does not make antibodies against our own antigens. This prevents an agglutination reaction in the body which is dangerous and can be deadly so people usually have the opposite antibody/antibodies to what antigen is on the red blood cell to prevent this from occurring (3). For example, if a person is blood group A, they have the A antigen on their red blood cells and will have B antibodies in their plasma. If a person is O, they won’t have any antigens on their red blood cells but will have A and B antibodies in their plasma.
The story is not finished yet. You may be aware that blood types are also classified as either positive or negative eg. O (+) or B (-). So what does this mean?
The positive and negative refer to the presence or absence of another antigen known as the Rhesus antigen (or antigen D), named after the Rhesus monkey where it was first discovered (5). If a person has the RhD antigen on their red blood cells they are RhD (+). If they do not, they are RhD (-).
The antibodies for the Rh system work in a different way to the ABO system. Humans don’t produce naturally occurring antibodies to the RhD antigen, even if we don’t have the antigen on our red blood cells. This means that neither positive or negative blood will contain naturally occurring RhD antibodies. Agglutination reactions can occur however when a person who is a negative blood type gets exposed to positive blood, either after a blood transfusion or for females during pregnancy (5).
The diagram below shows the different blood types and the antigens and naturally occurring antibodies present for each.
So how does this compare to blood types in our furry friends?
Have you ever wondered if dogs have blood types and if so, what your dog’s blood type is?
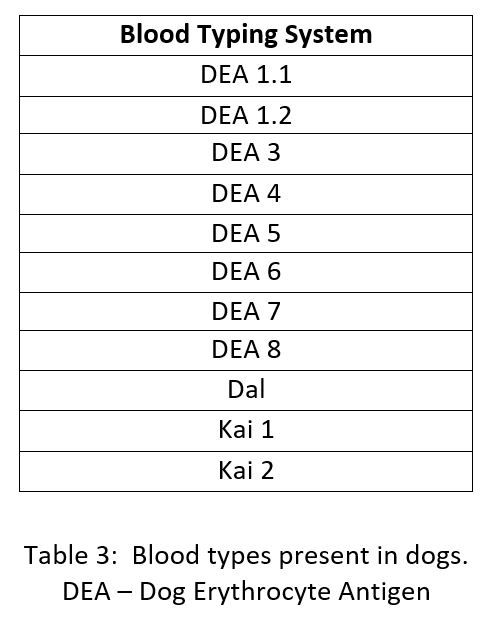
In dogs, the blood typing system is more complex with more than 12 blood group systems being identified (6).
If a dog contains the antigen on its surface it is positive for that system, and if it does not it is negative. Due to the inheritance of blood groups in dogs, they can contain a combination of all or some of the antigens on their red blood cells (7). For example, a dog may be DEA 1.1 (+), DEA 5 (-), Dal (+), Kai 1 (+) and Kai 2 (-).
Dogs only have naturally occurring antibodies for the DEA 3, DEA 5 and DEA 7 systems, and even then, only certain dogs will have them. These antibodies will also not cause severe reactions if they come into contact with their respective antigens, so are not as important as the naturally occurring antibodies found in humans (8).
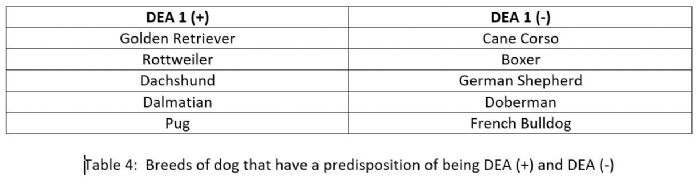
The blood group system DEA 1 (both DEA 1.1 and DEA 1.2) is the most important because approximately half the dog population is DEA 1 positive and the other half DEA 1 negative. It also has the highest antigenicity, meaning that if a DEA 1 antibody comes into contact with a DEA 1 antigen, it has the greatest ability to bind and cause a reaction (6). Some breeds have a predisposition to being either DEA 1 (+) or DEA 1 (-), as shown in the table below (6,9).
For the rest of this discussion we will focus on the DEA 1 system as it is the most important when considering blood transfusions.
Now that we have described the blood grouping systems in both humans and dogs, why is it important to know these blood types?
Both humans and dogs may require blood transfusions if they are ill or suffer an injury. It is important to give the patient the correct blood with the correct blood type, so an adverse reaction does not occur. As mentioned earlier, blood is composed of red blood cells and plasma, meaning that if a whole blood transfusion occurs, the recipient will receive both the red blood cells with specific antigens, as well as the antibodies in the plasma. This is not common practice, and generally only the red blood cells of the donor are given as there is greater chance for matching. For simplicity we will focus on just red blood cell transfusions (10).
First let’s look at human blood transfusions.
A haemolytic reaction occurs when a person is given the wrong blood and their own antibodies attack the transfused red blood cells. These reactions cause the bursting (lysis) of red blood cells and clumping of red blood cells. The destroyed red blood cells can cause blockages of small blood vessels, and therefore block the delivery of oxygen to tissues such as the brain and the heart, and may result in irreversible damage. This has a very dangerous effect on the patient and can be life threatening.
For example, if a person has the blood type A (-), they have A antigens on their red blood cells and B antibodies in their plasma. If this person needed a transfusion, we would need to ensure that the donor red blood cells do not possess any B antigens, as the recipients own B antibodies would attack and cause a haemolytic reaction.
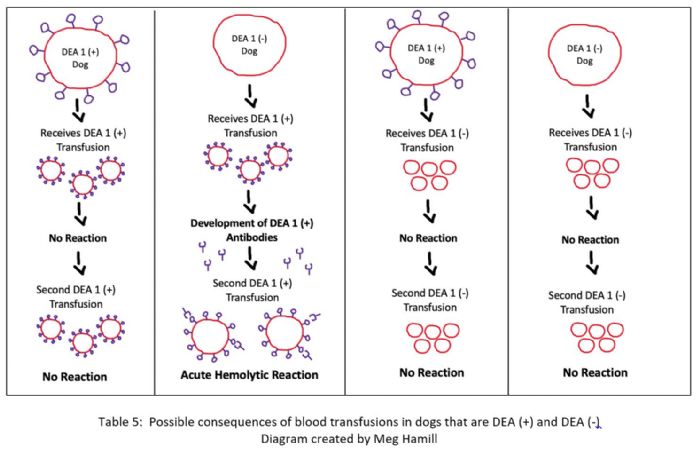
In dogs, the process is slightly different due to their lack of naturally occurring DEA 1 antibodies in the plasma. It does not matter what the dogs DEA 1 blood type is, nor what DEA 1 blood they receive via transfusion, no combinations will induce an acute haemolytic reaction. It is only after a secondary transfusion that issues could arise. This will only occur for one combination, if a DEA 1 (-) dog receives two DEA (+) transfusions. This is because after the first introduction of DEA (+) blood, the dogs immune system begins to develop antibodies against the foreign DEA 1 antigen. Once the immune system recognizes a foreign molecule, in this case an antigen, it will continue to produce the antibody, even after the foreign particle has been eliminated. When this blood is then reintroduced, the antibodies produced will immediately recognize the DEA 1 antigen on the new red blood cells. The antibodies will attach, and a haemolytic reaction will occur. This means that DEA 1 (+) dogs can receive either blood type, however DEA 1 (-) dogs can only receive DEA 1 (-) blood, making DEA 1 (-) dog’s universal donors (7).
These processes are shown in the diagram below.
The process seen in dogs can also be seen in humans in relation to the Rh system as we don’t possess naturally occurring antibodies to the RhD antigen. If a RhD (-) person receives blood that is RhD (+), the body will create antibodies against the antigen which will attack the red blood cells of any subsequent RhD (+) transfusions.
This mechanism is especially important in humans when considering pregnancy. If a RhD (-) mother is pregnant with a RhD (+) baby, during delivery some of the baby’s blood will mix with the mothers. There is no problem for the baby in the first pregnancy, however the mother’s body has recognized the RhD antigens and will produce RhD antibodies against them. If the mother becomes pregnant once again with a RhD (+) baby, the antibodies previously produced will attack the baby’s red blood cells and can cause haemolytic disease in the fetus which can be fatal (5). To prevent the risk of this occurring, if the mother is known to be RhD (-), they can receive an injection that stops the antibodies from attacking the babies red blood cells. If they give birth to a RhD positive baby, they will receive a second dose to prevent them from developing further antibodies (11).
The diagram below outlines this process.
In dogs this reaction does not occur in pregnancy. Female dogs that are DEA 1.1 negative are not usually exposed to the antigens of their puppies during pregnancy even if those puppies are DEA 1.1 positive. Even after the puppy is born this seems to be extremely rare. Most dogs pass on their antibodies to their puppies in the first milk called the colostrum. While a female dog that is DEA1.1 negative may have had a blood transfusion and develop antibodies to DEA1 1 positive this appears to be extremely rare that these antibodies are passed on to the puppy in colostrum milk.
What now?
Although it is helpful to know both your dogs and your own blood type, before any transfusion, the doctor or veterinarian will complete a major crossmatch in which the washed red blood cells from the donor are mixed with the plasma of the recipient to ensure no agglutination reaction will occur (7). In dogs, the overall reported incidence of transfusion reactions ranges from 5-25%, and in humans the incidence of an acute haemolytic reaction is 1:76,000, so reactions are very rare (12, 13).
Acknowledgements: We thank Dr Steve Holloway and Prof Brian Corbitt for comments on the article.
References
- Fairview [internet]. Minnesota: Fairview Health; c2019. Understanding Blood and Blood Components. N.d. [cited 2021 Oct 1]; [about 3 screens]. Available from: https://www.fairview.org/Patient-Education/Articles/English/u/n/d/e/r/Understanding_Blood_and_Blood_Components_40309
- -
- Dean L. Blood Groups and Red Cell Antigens [internet]. Bethesda: National Center for Biotechnology Information (US); c2005. Chapter 2, Blood group antigens are surface markers on the red blood cell membrane; [cited 2021 Sept 19]; [about 5 screens]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2264/
- Lumen Learning. Agglutination Assays [internet]. 2020 [cited Oct 1]. Available from: https://courses.lumenlearning.com/microbiology/chapter/agglutination-assays/
- The Editors of Encyclopedia Britannica. Rh Blood Group System [internet]. Britannica. 2020 April 9 [cited 2021 Oct 7]; [about 3 screens]. Available from: https://www.britannica.com/science/Rh-blood-group-system
- Ebelt A K, Funchs S, Weber C, Müller E, Giger U. Survey of Blood Groups DEA 1, DEA 4, DEA 5, Dal, and Kai 1/ Kai 2 in Different Canine Breeds from a Diagnostic Laboratory in Germany. Front. Vet. Sci [internet]. 2020 Feb 28 [cited 2021 Sept 19]; 7(85): 10 pp. Available from doi: 10.3389/fvets.2020.00085
- Cotter S. MSD Veterinary Manual [internet]. New Jersey: Merck Sharp & Dohme Corp; c.2021. Blood Groups and Blood Transfusions in Dogs. 2017 Dec [cited 2021 Sept 19]; [about 2 screens]. Available from: https://www.msdvetmanual.com/dog-owners/blood-disorders-of-dogs/blood-groups-and-blood-transfusions-in-dogs#
- Eclinpath [internet]. Cornell: Cornell University College of Veterinary Medicine; c.2013-2020. Blood Types. N.d. [cited 2021 Sept 19]; [about 5 screens]. Available from: https://eclinpath.com/hemostasis/transfusion-medicine/blood-types/
- Valentin A A M, Gavazza A, Lubas G. Prevalence of Dog Erythrocyte Antigen 1 in 7,414 Dogs in Italy. Vet Med Int. [internet]. 2017 Sept 24 [cited 2021 Oct 7]; 5914629: 10 pp. Available from doi: 10.1155/2017/5914629
- Mayo Clinic [internet]. Minnesota: Mayo Foundation for Medical Education and Research; c.1998-2021. Blood Transfusion. 2021 April 15 [cited 2021 Sept 20]; [about 4 screens]. Available from: https://www.mayoclinic.org/tests-procedures/blood-transfusion/about/pac-20385168
- University of Rochester Medical Centre [internet]. Rochestor, University of Rochester Medical Centre; c.2021. Hemolytic Disease of the Newborn (HDN). N.d. [cited 2021 Oct 7]; [about 6 screens]. Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=90&ContentID=P02368
- Barnette C. VCA [internet]. California: VCA Hospitals; c.2021. Blood Transfusion Reactions in Dogs. N.d. [cited 2021 Oct 7]; [about 4 screens]. Available from: https://vcahospitals.com/know-your-pet/blood-transfusion-reactions-in-dogs
- Australia Red Cross Lifeblood [internet]. Australia Red Cross Lifeblood; c.2019. Classification and incidence of adverse effects. 2020 Nov 25 [cited 2021 Oct 7]; [about 1 screen]. Available from: https://transfusion.com.au/adverse_transfusion_reactions/classification_and_incidence
Contact Details
Chair Sue Anderson Liaison Officer: A FullerSeaford, VIC, Australia